- Home
- Common Knee Conditions
- ITB Syndrome
Iliotibial Band Syndrome
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board
Iliotibial Band Syndrome (ITBS) is one of the most common injuries seen in runners, especially long distance runners.
ITBS causes lateral knee pain on the outer side of the knee, which can radiate up the thigh and is notoriously difficult to treat.
Also known as Iliotibial Friction Syndrome, ITB syndrome or ITBS, it is often misdiagnosed as Runners Knee.
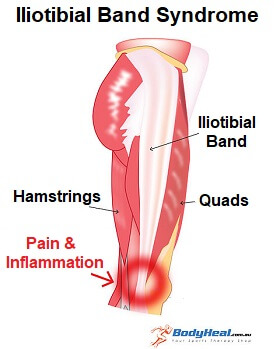
The Iliotibial Band, aka IT Band, is a thick band of fibrous tissue, rather than a muscle, that runs down the outside of your leg from your pelvis to your knee. It has a different structure to muscles, making it less mobile and harder to stretch.
Some of the buttock and hip muscles attach to the ITB, and it co-ordinates how these muscles work as well as stabilising the knee and leg.
Here we will look at the typical causes and symptoms of ITBS, the best treatment options, and how to reduce the chances of developing ITBS.
What Is Iliotibial Band Syndrome?
Iliotibial Band Syndrome develops when the IT Band gets irritated and inflamed due to friction. This most commonly occurs at the bottom of the band where it inserts on the outer side of the knee.
As the leg bends and straightens, the IT Band glides over a bony lump on the side of the knee that sticks out slightly, called the lateral epicondyle.
A bursa (small fluid filled sac) sits
between the ITB and the bone to allow smooth, gliding movements, but if
there is too much friction, the Iliotibial Band gets irritated. When it
is irritated, friction from walking and running can cause inflammation
and pain to develop.
Inflammation of the IT Band usually occurs from overuse and is most commonly seen in runners, especially those who do long distance running.
What Causes IT Band Pain?
Common causes and risk factors for iliotibial band syndrome are:
- Running: Long distance running can also lead to Iliotibial band syndrome due to repetitive friction. Lots of running surfaces e.g. roads and running tracks are slightly banked which places more of a stretch through the ITB on the lower leg. Running up and down hills also puts even more tension through the IT Band.
- Muscle Problems: Tightness in the leg muscles and the Iliotibial Band itself increases the friction on the ITB. Weakness in the buttock muscles (glutes) puts more strain on the Iliotibial Band, increasing your chances of developing Iliotibial Band Syndrome.
- Sudden Increase in Activity: Someone who rapidly increases their training is at risk of developing Iliotibial Band Syndrome due to the sudden increase in friction at the knee.
- Altered Foot Biomechanics: Anything which changes the normal position of the leg can place more strain through the IT Band. If you have flat feet, a leg length discrepancy or bowed legs you are more prone to developing ITB syndrome.
- Bone Spurs: If there are small lumps of extra bone, known as bone spurs or osteophytes, around the attachment of the ITB, it causes excess friction on the ITB which can lead to ITBS.
Symptoms of IT Band Syndrome
The main symptoms of Iliotibial Band Syndrome are:
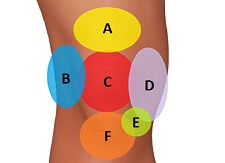
- Lateral Knee Pain:
pain over the outer side of the knee, especially when the heel strikes
the floor. Outer knee pain from iliotibail band syndrome is typically worse with running and stairs, especially when
going down. It may also hurt to bend and straighten the knee.
- Knee Swelling: on the outer knee due to inflammation or thickening of the Iliotibial band.
- Popping/Snapping Sensation: there may be some knee pain and popping when you bend the knee as the IT Band flicks over the lateral epicondyle.
ITB Syndrome Treatment
As with any overuse injury, it is really important to work out what caused the Iliotibial band to become inflamed in the first place. A physical therapist/sports injury specialist should be able to assess this for you. It can take several weeks/months to recover fully from Iliotibial Band Syndrome.
#CommissionsEarned from Amazon on qualifying purchases
Short Term Treatment
The initial aim of iliotibial band syndrome treatment is to reduce the inflammation which will in turn also reduce the IT band pain. This is most effectively done using:

- Relative Rest: It is really important to rest initially with iliotibial band symdrome. Avoid aggravating activities to give the ITB time to heal else you will slow down your recovery. The mantra “No pain, no gain” does NOT
apply here! LEARN MORE >
- Regular Ice: Ice therapy can be used to help reduce inflammation, but only when used correctly. In the Ice Treatment section we look at how to get the maximum benefit from using ice and the best ways to apply ice. LEARN MORE >
- Take Anti-Inflammatories: Medications such as ibuprofen/Advil can be really helpful in reducing pain and inflammation with ITB syndrome.
- Switch Sports: If your symptoms are aggravated by running, you might find that switching to activities like swimming or cycling allow you to keep exercising without aggravating the Iliotibial Band.
Longer Term Treatment
Long term treatment aims to address the cause of the Iliotibial Band Syndrome and may include:
- Wear A Knee Strap: Wearing a brace that straps around the top of the knee directs forces away from the Iliotibial band so can be very helpful to reduce irritation when running. Many runners swear by them! FIND OUT MORE >
- Do Strengthening IT Band Exercises: Strengthening exercises are a vital part of iliotibial band syndrome treatment. Strengthening the glutes, quads and hamstrings improves how the hip and knee function which reduces the friction on the Iliotibial Band. FIND OUT MORE >
- Start Stretches for IT Band: The best place to start is with IT band stretches, but should not be done in isolation. Stretching the quads, hamstrings and calf muscles also helps reduce the friction at the knee. FIND OUT MORE >
- Try Taping: Taping can also be used to reduce the forces going through the IT Band – your physical therapist/ sports injury specialist will show you what to do and then you can do it yourself at home
- Have a Sports Massage: Deep tissue massage to the IT Band can reduce tightness, but it can be quite painful. It should be carried out by a trained sports therapist or physical therapist and should be followed up with an exercise programme. Alternatively you can use a massage gun at home to help stretch out the ITB.
- Steroid Injections: If other treatments have failed, a cortisone injection can be given to help reduce pain and inflammation. However it should always be accompanied by strengthening and stretching exercises to ensure the problem doesn’t return. LEARN MORE >
- Surgery: Surgery for IT Band pain is extremely rare and is only considered if all other treatments have failed. It is done arthroscopically, keyhole surgery, and aims to break down any scarring in the tissues and if necessary lengthen the Iliotibial band to reduce the friction at the knee.
- Try Orthotics In Your Shoes: Special insoles can be worn in your shoes to correct poor foot positions such as flat feet and thus take the tension of the ITB. See an orthotist for a full assessment and advice.
How To Prevent IT Band Syndrome
The most common cause of Iliotibial Band Syndrome is running. To help prevent IT Band syndrome from developing or recurring:
- Warm Up and Cool Down Properly: including stretching. Visit the stretching section for guidance on how to stretch effectively - most people don’t stretch properly.
- Wear Good Running Shoes: And change them regularly
- Wear Orthotics If Required: Shoe inserts to correct any abnormal foot positions or leg length discrepancies
- Avoid Training Errors: such as avoiding running in the same direction on banked surfaces and slowly increasing distances.
What Else Can Help?
There are a number of other causes of lateral knee pain as well as Iliotibial Band syndrome.
If this doesn’t sound quite like your problem, visit the knee pain diagnosis section for help working out what is wrong with your leg.
You may also be interested in the following articles:
- Inner Knee Pain
- Front Knee Pain
- Pain Behind The Knee
- Side Knee Swelling
- How To Do Stairs With Knee Pain
- Knee Pain Diagnosis Chart
Related Articles
Last Updated: September 10th, 2025
Next Review Due: September 10th 2027