- Home
- Hip Pain Diagnosis
- SPD Pelvic Pain
Symphysis Pubis Dysfunction (SPD)
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board

Symphysis pubis dysfunction is a condition that causes pain and instability at the front of the pelvis.
It is particularly common during pregnancy but can also occur in athletes and individuals with pelvic trauma or biomechanical issues.
Pubic symphysis pain can significantly affect mobility and quality of life, especially when walking, climbing stairs, or turning over in bed.
In this article, we’ll explore what symphysis pubis dysfunction is, where the pain comes from, why it happens, what symptoms to look out for, how it’s diagnosed and treated, and what you can do to help prevent it.
What Is Symphysis Pubis Dysfunction?
Symphysis pubis dysfunction is a condition involving excessive movement or instability at the front of the pelvis. It is also known as SPD, pubic symphysis dysfunction, or pubis symphysis dysfunction.
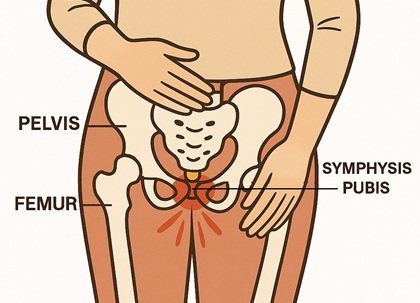
The pubic symphysis is the cartilaginous joint at the center front of the pelvis, where the two halves of the pelvic bone meet, just above the genitals.
The joint is supported by a network of strong ligaments and is surrounded by muscles such as the hip adductors, abdominals and pelvic floor.
The pubic symphysis allows for a small amount of movement, typically around 2–3mm, to aid with activities such as walking and twisting, and plays a crucial role in stabilising the pelvis and absorbing forces during activities.
With symphysis pubis dysfunction, the joint becomes excessively mobile, misaligned or inflamed, often due to hormonal, mechanical, or biomechanical changes. The result is sharp or aching pain in the pubic region, instability, and difficulty with normal movement.
During pregnancy, hormonal changes increase the laxity of the ligaments around this pubic symphysis to allow for your pelvis to expand as the fetus grows, but in some cases, this can lead to pain and dysfunction. Symphysis pubis pain affects around 25% of women during pregnancy and is just one possible cause of pelvic and inner thigh pain.
What Causes Symphysis
Pubis Dysfunction?
Pubic symphysis dysfunction is most commonly associated with pregnancy, especially in the second and third trimester, but can affect anyone. Common causes include:
- Hormonal changes in pregnancy increase the laxity of the pelvic ligaments around the joint to allow for delivery. Your body may start producing the hormone relaxin as early as 10 weeks into pregnancy.
- Weight gain, changes in posture and pelvic instability due to the growing uterus alter the load on the pelvis and shift the center of gravity
- Trauma to the pelvis, such as from a fall, high-impact sports injury, or car accident
- Post-surgical changes, especially after pelvic or abdominal procedures
- Muscle imbalances, particularly weak or tight abdominal, gluteal, and adductor muscles
- Hypermobile joints, particularly in individuals with generalised joint laxity e.g. Ehlers-Danlos Syndrome
- Biomechanical issues, such as poor posture, leg length discrepancy, altered gait or uneven loading through the pelvis (e.g. carrying a toddler on one hip) can place strain on the pubic symphysis.
Some women may be more predisposed to symphysis pubis dysfunction in pregnancy due to pre-existing pelvic asymmetry, previous pelvic trauma, or a history of lower back pain.
Symphysis Pubis Dysfunction Symptoms
Symptoms of pubic symphysis dysfunction can vary from mild to severe and may affect one or both sides of the pelvis. Common symptoms of SPD include:
- Pain at the front of the pelvis, especially directly over the pubic bone, that may radiate into the groin, hips, inner thighs, lower abdomen or lower back
- Worsening pain with activities where your legs move apart e.g. walking, climbing stairs, getting in/out of bed or a car or standing on one leg
- A feeling of instability in the pelvis
- Clicking, grinding, or popping sensations in the pelvic area, especially with movement
- Pain during sexual intercourse
- Difficulty sleeping, due to hip pain at night, particularly when rolloing over
The discomfort can range from mild discomfort to sharp, stabbing pain that affects daily life. It often worsens as the pregnancy progresses and the pelvis prepares for birth. Symphysis pubis pain may persist postpartum if not properly addressed.
Diagnosing Pubic Symphysis Dysfunction
Diagnosis of symphysis pubis dysfunction involves a detailed clinical assessment, often supported by imaging if needed.
A healthcare provider, usually a physiotherapist or obstetrician, will:
- Review your symptoms and history, including pregnancy stage, physical activity, previous injuries, or pelvic surgeries
- Palpate the pubic symphysis and surrounding muscles for tenderness
- Perform specific tests, such as the active straight leg raise or single-leg stance, to assess pelvic stability and reproduce symptoms
- Evaluate posture, gait, and pelvic alignment
Although not always required, imaging may help in severe or unclear cases:

- X-rays can detect increased pubic symphysis separation, especially postpartum. A gap more than 10mm between the pubic bones indicates pubic symphysis instability
- MRI provides detailed images of joint inflammation and soft tissue involvement
- Ultrasound may be used to measure separation of the joint or guide treatment
Differential Diagnosis
Several other conditions can mimic symphysis pubis dysfunction, including:
- Pelvic Girdle Pain (PGP): a broader term where multiple pelvic joints are affected including the sacroiliac joint
- Groin strain or adductor tendinopathy
- Osteitis pubis: inflammation of the pubic symphysis due to overuse or trauma
- Inguinal hernia
- Hip joint issues, such as labral tears or impingement
- Urinary tract or gynaecological conditions
A thorough assessment is crucial to differentiate pubis symphysis dysfunction from these and guide appropriate treatment.
Treatment for Symphysis Pubis Dysfunction
Symphysis pubis dysfunction treatment focuses on relieving pain, stabilising the pelvis, and improving function and usually involves a combination of:
1. Physical Therapy
A tailored physical therapy programme is key to successful recovery from pubic symphysis dysfunction and may include:
- Pelvic stability exercises, such as core activation, pelvic floor strengthening, pelvic tilts, and glute strengthening
- Stretching tight areas like hip flexors or inner thighs
- Manual therapy to address joint restrictions and muscle imbalances
- Postural re-education and advice on safe movement strategies
- Functional retraining, including how to move, lift, and roll out of bed with minimal pain
2. Pelvic Support Belts

A maternity support belt or pelvic brace can help stabilise the joint and reduce pubic symphysis pain in pregnancy during movement.
Some consist of a single strap, whereas others have an extra strap that goes around the top of your baby bump.
3. Pain Relief
Ice or heat therapy can reduce symphysis pubis pain and inflammation and ease muscle tension
Paracetamol is typically the first-line medication during pregnancy. Anti-inflammatories (NSAIDs) may be used with caution postpartum or under medical advice
4. Modifying Activities
Avoid aggravating movements such as wide-leg positions, deep squats, or prolonged standing.
Try to keep both legs together during activities such as getting in and out of the car or rolling over in bed. Use a pillow between your knees when sleeping and keep movements symmetrical when possible.
Check out our Amazon Storefront to find the best knee pillows to prevent hip and pelvis pain in bed.

#CommissionsEarned from Amazon on qualifying purchases
5. Surgery (Rare)
In severe or unresponsive cases, particularly post-trauma or postpartum, surgical stabilisation of the pubic symphysis may be considered. This is very rare and typically reserved for persistent cases that fail to respond to conservative care.
Recovery Process
The recovery timeline for symphysis pubis dysfunction can vary depending on the underlying cause and the individual’s overall health. With early intervention, most people see significant improvement within a few weeks to a few months.
- During Pregnancy: Symptoms of SPD often improve or resolve after childbirth, although they may persist for several months postpartum. The ligaments will start to tighten up once your body stops producing relaxin and you will regain the stability in your pelvis
- Non-Pregnancy Cases: Most improve within 6–12 weeks with consistent physiotherapy and activity modification
- Chronic Cases: May require longer rehabilitation and multi-disciplinary input
Commitment to rehab exercises, proper pelvic support, and lifestyle adjustments are crucial to a successful recovery.
What Activities Should You Avoid with SPD?
Certain everyday activities can aggravate symphysis pubis dysfunction by placing uneven stress on the pelvis, so try to limit or avoid the following:
- Standing: avoid standing with you weight on one leg e.g. when dressing or carrying a child on one hip, and avoid standing for too long
- Lifting: avoid twisting or bending when lifting objects, and avoid lifting anything heavy e.g. laundry baskets, shopping bags, toddlers
- Sitting: avoid crossing your legs when sitting, sitting on the floor, sitting in a twisted position, or sitting for prolonged periods
- Activities: avoid vacuuming or pushing heavy objects like a shopping cart, and avoid carrying anything with one hand instead of evenly distributing the weight
Making small adjustments to how you move and carry things can help protect your pelvis and reduce pubic symphysis pain.
How to Avoid SPD
While some risk factors for symphysis pubis dysfunction, such as pregnancy hormones, are unavoidable, there are still steps you can take to reduce your risk:
- Stay active during pregnancy with gentle, low-impact exercise like walking, swimming, or prenatal yoga, as long as they don’t aggravate your symptoms
- Strengthen your core and glutes to improve pelvic stability
- Avoid heavy lifting or activities that cause pelvic strain
- Maintain good posture, especially when sitting or standing for long periods
- Avoid standing on one leg e.g. putting pants on while standing
- Wear comfortable, supportive footwear to promote even weight distribution - avoid high heels and flip-flops
- Consider wearing a pelvic support belt during late pregnancy or if at high risk
Being proactive with pelvic health before and during pregnancy can make a big difference in preventing or reducing pubic symphysis dysfunction pregnancy symptoms, particularly if you suffered from SPD in a previous pregnancy
FAQ’s on SPD
What Does Symphysis Pubis Dysfunction Feel Like?
What Does Symphysis Pubis Dysfunction Feel Like?
Symphysis pubis dysfunction usually feels like a sharp, stabbing, or burning pain at the front of the pelvis, near the pubic bone. The pain may radiate into the groin, hips, thighs, or lower back and is often worse when walking, going upstairs, rolling over in bed, or standing on one leg.
How Early In Pregnancy Can You Get SPD?
How Early In Pregnancy Can You Get SPD?
Symphysis pubis dysfunction can develop at any point during pregnancy but is most common in the second or third trimester as hormone levels rise and pelvic changes become more pronounced. However, some women experience symptoms as early as the first trimester.
Why Is Pubic Symphysis Dysfunction Worse At Night?
Why Is Pubic Symphysis Dysfunction Worse At Night?
SPD often worsens at night due to a combination of fatigue, hormonal effects, and sleeping positions. Ligaments are naturally more lax during pregnancy due to the hormone relaxin, and lying on your side can put asymmetrical pressure on the pelvis. Additionally, reduced movement during the night can cause stiffness and increased discomfort when turning over in bed.
How Do I Sleep With Symphysis
Pubis Pain?
How Do I Sleep With Symphysis Pubis Pain?
Try sleeping with a pillow between your knees and ankles to keep your pelvis aligned. A supportive mattress or mattress topper may also help. Avoid sleeping on your back in later pregnancy, and roll over with your knees together to reduce strain on the pelvis.
Is
SPD The Same As Pelvic Girdle Pain (PGP)?
Is SPD The Same As Pelvic Girdle Pain (PGP)?
Symphysis pubis dysfunction is a type of pelvic girdle pain. PGP is a broader term that includes dysfunction of the sacroiliac joints as well as the pubic symphysis. SPD refers specifically to problems at the front of the pelvis.
Can SPD Get Worse As Pregnancy Progresses?
Can SPD Get Worse As Pregnancy Progresses?
Yes, symphysis pubis dysfunction in pregnancy often worsens in the second and third trimesters as the pelvis loosens more and the baby grows. The additional weight and changes in posture and gait increase the strain on the pelvic joints leading to pubic symphysis pain.
Is Walking Bad For Symphysis Pubis Dysfunction?
Is Walking Bad For Symphysis Pubis Dysfunction?
Walking can aggravate pubic symphysis dysfunction symptoms, especially if done for long periods or on uneven surfaces. Short, slow walks may still be beneficial, but it is important to listen to your body and avoid overdoing it. A support belt may help improve comfort during walking.
Is It Safe To Exercise With SPD?
Is It Safe To Exercise With SPD?
Yes, gentle, low-impact exercise guided by a physiotherapist can be very beneficial with pubis symphysis dysfunction in pregnancy. Avoid high-impact movements, single-leg exercises, and wide stances. Focus on strengthening your core, glutes, and pelvic floor.
Can SPD Cause Permanent
Damage?
Can SPD Cause Permanent Damage?
Symphysis pubis dysfunction typically resolves after birth, especially with proper treatment. In rare cases, symptoms may persist postpartum. With physiotherapy and pelvic rehabilitation, long-term damage is unlikely. However, untreated SPD can lead to chronic pelvic instability or pain.
Can I Still Give Birth Naturally With SPD?
Can I Still Give Birth Naturally With SPD?
Yes, many women with symphysis pubis dysfunction have successful vaginal births. However, it is important to inform your midwife or obstetrician so they can avoid positions that overly strain the pelvis. Water births or side-lying positions may be more comfortable. And the good news is, pubic symphysis dysfunction does not hurt the baby, during pregnancy or birth.
Does Symphysis Pubis
Dysfunction Go Away After Pregnancy?
Does Symphysis Pubis Dysfunction Go Away After Pregnancy?
For most women, pubic symphysis dysfunction pregnancy symptoms improve within a few weeks postpartum. Some may need ongoing physiotherapy to fully recover, especially if symptoms persist beyond 12 weeks. Continuing rehab exercises after birth can help speed up recovery.
Pubic Symphysis Dysfunction Summary
Symphysis pubis dysfunction is a common but manageable condition that causes pain and instability at the front of the pelvis. It most frequently affects women during pregnancy but can also occur due to injury or biomechanical stress.
Early diagnosis and a structured management plan, including physiotherapy, pain relief, and lifestyle adjustments, can lead to full recovery and better quality of life.
If you are struggling with pubic symphysis pain, especially during pregnancy, don’t ignore it, the right care can make a huge difference in your comfort and mobility.
You may also be interested in the following articles:
- Inner Thigh Pain
- Front Hip Pain
- Groin Strain
- Osteitis Pubis
- Snapping Hip Syndrome
- Glute Strengthening Exercises
- Knee Pain Diagnosis Chart
Related Articles
Hip Pain At Night
October 2nd, 2025
Hip Pain Diagnosis
September 16, 2025
Hip Strengthening
September 24, 2025
Medical & Scientific References
- Management of Symphysis Pubis Dysfunction During Pregnancy Using Exercise and Pelvic Support Belts. Physical Therapy & Rehabilitation Journal
- Postpartum Pubic Symphysis Diastasis. National Library Of Medicine
- Pubic Diastasis. Radiopaedia
- Management Of Symphysial Dysfunction In Pregnancy And Post-Partum Period: A Review. Sri Lanka Journal Of Obstetrics & Gynaecology
Last Updated: September 19th, 2025
Next Review Due: September 19th, 2027