- Home
- Common Knee Conditions
- Osteochondritis Dissecans
Osteochondritis Dissecans
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board
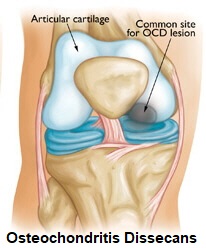
Osteochondritis Dissecans is a joint condition where loose fragments of bone and cartilage break off the end of a bone.
This is typically triggered by a lack of blood flow to the bone.
Osteochondritis most commonly affects the knee (75% of cases) but can also affect the elbow, ankle, shoulder, hand, wrist or hip.
Typical symptoms include are pain, locking, clunking, weakness, stiffness and swelling.
Osteochondritis usually affects people between the ages of 10-20 years and is three times more common in men than women. It tends to develop in people who do repetitive actions that involve lots of knee movement such as jumping.
Here we will look at how osteochondritis dissecans develops including the causes, symptoms, diagnosis and best treatment options for it, focusing on how it affects the knee joint.
What Is Osteochondritis?
Osteochondritis Dissecans (OCD) is a condition where fragments of bone and cartilage become detached and break off from the joint.
The way the disease generally develops is:
- Lack of Blood Supply: When there is inadequate blood flow, the bone and cartilage can become ischemic, meaning it doesn't receive enough oxygen and nutrients. This starves the bone of vital nutrients and can lead to cell death, particularly in the bone tissue, which is known as avascular necrosis
- Fragment Formation: As a result of avascular necrosis, the bone starts to degenerate. Thin layers of bone and the adjoining cartilage lose their structural integrity and come loose. Over time, they may break off completely. Bone fragments can vary in size and shape, and are commonly referred to as an "osteochondral lesion"
- Inflammatory Response: The separation of bone and cartilage can trigger an inflammatory response within the joint
If left untreated, osteochondritis dissecans of the knee can lead to the progression of joint degeneration over time. This can result in long-term joint damage, including osteoarthritis, which is characterized by the gradual erosion of joint surfaces and ongoing pain and stiffness.
What Causes Knee Osteochondritis?
The exact cause of knee osteochondritis dissecans is not always clear. Several contributing factors are believed to play a role reducing the blood supply to the bone and the development of osteochondritis in the knee:
- Repetitive Microtrauma: Repetitive stress or minor trauma to the affected joint is a common trigger for osteochondritis dissecans. This This usually happens with activities that involve high-impact or repetitive motions, such as running, jumping or rapid changes in direction
- Genetic Predisposition: Some individuals may have a genetic predisposition to developing osteochondritis. If there is a family history of the condition, it may increase the likelihood of its occurrence. There is a genetic link in about 10% of cases
- Hormonal Factors: In some cases, hormonal imbalances or changes, such as those that occur during adolescence, may influence the development of knee osteochondritis dissecans. This is why it is more common in teenagers and young adults
- Joint Instability: Joint instability, which can result from ligament injuries or laxity, may also contribute to the development of OCD. Unstable joints can lead to increased stress on certain areas, increasing the risk of the separation of bone and cartilage
- Overuse and Over-training: Engaging in repetitive, high-impact activities without adequate rest and recovery can increase the risk of osteochondritis dissecans. Athletes who overtrain or specialize in one sport may be more susceptible
- Trauma: Acute trauma to the knee, such as a direct blow or injury, can also be a triggering factor for OCD. A single traumatic event can damage the blood vessels supplying the bone and cartilage
Where Does Osteochondritis Occur?
Osteochondritis Dissecans most commonly happens at the knee accounting for 75% of all cases.
80% of knee lesions occur on the medial side of the knee (inner side) as it takes more weight than the outer side.
The next most common sites for Osteochondritis are the ankle and elbow, and very occasionally it develops in the shoulder, hand, wrist or hip.
It can be bilateral (affects both left and right side) in 20-30% of cases, and sometimes it affects more than one joint at the same time. It is a rare disease with approximately 3-6 cases per 10,000 people.
Common Symptoms
The most common symptoms of Osteochondritis Dissecans at the knee are:
- Pain: is the most common symptom of osteochondritis dissecans and tends to be triggered by activities such
as stairs, sports and any twisting movements. It tends to develop
gradually and is a vague, achy pain, but people sometimes get a sharp,
stabbing pain if the loose fragment gets stuck
- Joint Locking: in some cases the knee joint may "catch" or "lock" if the loose fragment gets stuck in the joint.
You might have to wiggle your leg to move the fragment before you can
then straighten the knee
- Swelling: knee swellling is a common symptom of osteochondritis dissecans. The loose fragment can cause irritation and inflammation in the joint, leading to fluid accumulation and swelling
- Weakness & Instability: the leg may feel like it “gives way” or is weak. This typically gets worse over time as the muscles start to waste from lack of use due to pain
- Decreased Movement: knee range of motion may be affected and the knee may not be able to fully bend and/or straighten, especially if there is a loose fragment
- Clunking: There may be a painful “clunk” when bending or straightening the knee. This usually happens when the outer side (lateral) of the knee is affected.
Diagnosing Osteochondritis
Osteochondritis dissecans (OCD) is typically diagnosed through a combination of clinical evaluation, imaging studies, and sometimes additional tests:
- X-rays: show changes in the bone and any loose fragments
- CT scan: shows cartilage and bone. Helps show the exact location of any loose bodies
- MRI scans: show more detailed images showing the size, quality and stability of any fragments. This helps determine whether surgery is indicated or whether it is likely to heal naturally
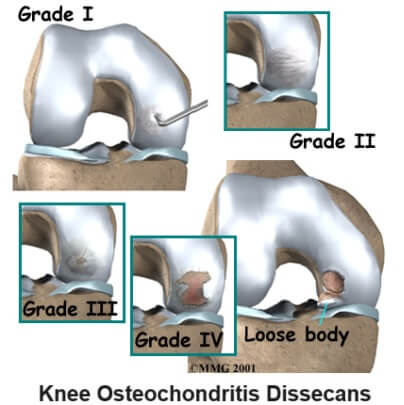
Osteochondritis Dissecans Stages
There are four stages of Osteochondritis Dissecans which can be seen most clearly on an MRI scan:
- Stage 1: Thickening of the articular cartilage and flattening of the subchondral bone. Stable.
- Stage 2: Subchondral cyst present and/or incomplete separation of a fragment. Stable.
- Stage 3: Incomplete separation with fluid around the undisplaced fragment. Unstable.
- Stage 4: Complete separation with a loose body. Unstable.
There are a number of other conditions that can present in a similar way to knee osteochondirits dissecans including:
Osteochondritis Dissecans Treatment
Treatment varies according to the severity of Osteochondritis Dissecans and the age and activity levels of the person affected but typically aims to:
- Reduce pain and swelling
- Repair the joint surface
- Decrease the chance of future problems e.g. Osteoarthritis
#CommissionsEarned from Amazon on qualifying purchases
Stage 1-2 osteochondritis dissecans lesions can usually be treated conservatively with:
- Rest:
avoid activities that stress the joint such as sports for 6-12 weeks to allows the bone to heal. Crutches may be required.
- Knee Braces: can be worn to help support the knee and reduce the pressure going through the joint. Usually an Advanced Knee Brace or Elite Brace will be of most benefit as they provide the right level of support to allow healing to occur.
- Physical Therapy: to strengthen and stretch the joint without aggravating the condition – see the knee strengthening exercises and knee stretches sections.
If the fragment stays put, it will often heal by itself with few or no symptoms. However, the fragment can come loose and move around in the joint causing pain and restricting movement. If this happens, surgery may be required.
Children and young adults tend to respond best to these treatments as their bones and cartilage are much better at regenerating. Most adults with Osteochondritis Dissecans will require surgery.
Surgical Treatment

If conservative treatment has failed, or if the osteochondritis dissecans has progressed to stage 3 or 4, surgery is usually required.
This is usually done arthroscopically (keyhole surgery) where a small camera and surgical tools are inserted into the joint through small holes.
An arthroscopy for osteochondritis dissecans may involve one or more of these techniques:
- Debridement: In some cases, especially if the fragment is loose and causing mechanical symptoms, the surgeon may perform arthroscopic debridement. This involves removing the loose fragment and smoothing the affected area
- Drilling or Microfracture: For smaller lesions where the fragment is still partially attached, the surgeon may use a minimally invasive approach to stimulate blood flow and improve the healing process. Drilling small holes in the bone or performing microfracture can promote the growth of new cartilage
- Fragment Fixation: In cases where the fragment is large and stable, the surgeon may reattach it to the bone using screws or pins. This can be performed arthroscopically or through open surgery
- Autologous Chondrocyte Implantation: ACI is a surgical procedure used for larger lesions. It involves the transplantation of healthy cartilage cells from the patient's own body to repair the damaged area.
- Osteochondral Allograft: In severe cases where the affected area is large and other treatments have failed, an osteochondral allograft involves transplanting a piece of donor cartilage and bone to replace the damaged tissue.
Following surgery for osteochondritis dissecans knee, pain and swelling can be controlled with ice and medication, usually a combination of painkillers e.g. paracetamol/acetaminophen and anti-inflammatories e.g. ibuprofen/Advil. It is very important to follow your rehab programme which may initially restrict how much you can use your knee.
Physical therapy can then be commenced with strengthening and stretching exercises to improve the stability and flexibility of the knee. Knee Braces are particularly useful after surgery to help the knee to help protect the knee and allow it to heal. It usually take 3-6 months to full recover from osteochondritis dissecans surgery.
What Else Can Help?
Osteochondritis Dissecans is extremely rare. If this isn’t sounding quite like your knee pain, visit the common knee conditions section to find out about other common causes of knee pain or visit the knee pain diagnosis section for help working out what is causing your knee pain. You may also be interested in the following articles:
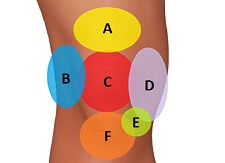
- Knee Pain Chart
- Front Knee Pain
- Inner Knee Pain
- Outer Knee Pain
- Pain Behind The Knee
- Swelling Above The Knee
- How To Do Stairs With Knee Pain
Page Last Updated: 10/01/24
Next Review Due: 10/01/26