- Home
- Hip Pain Diagnosis
- Hip Tendonitis
- Glute Tendonitis
Gluteal Tendinopathy
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board

Gluteal tendinopathy is one of the most common causes of outer hip pain.
It is caused by irritation or degeneration of the gluteal tendons on the outside of the hip, often affecting runners and middle-aged women.
Gluteal tendinitis is a condition that affects your ability to walk, sleep, and move comfortably, but with the right approach, it is absolutely treatable.
In this article, we’ll look at what gluteal tendinopathy is, the main causes and symptoms, how it is diagnosed, and the best ways to treat and manage it effectively, so you can get back to doing the things you love, pain-free.
What Is Gluteal Tendinopathy?
Gluteal tendinopathy, sometimes referred to as gluteal tendonitis or gluteal tendinitis, is a common cause of chronic outer hip pain. It is typically caused by irritation or degeneration of the gluteus medius and gluteus minimus tendons.
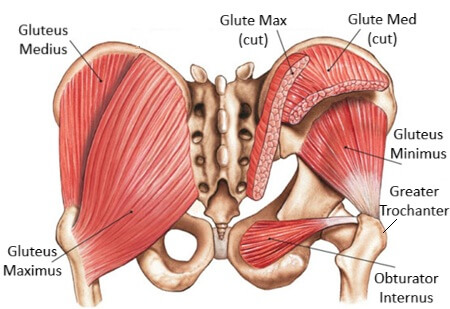
These two glute muscles sit on the outer surface of your pelvis and play a vital role in stabilising the hip and pelvis during walking, running, and standing on one leg.
Tendons are strong, thick, flexible bands that connect the hip muscles to bone. The glute tendons insert into a bony prominence on the outside of the thigh bone, called the greater trochanter. This is the exact spot where most people with gluteal tendinopathy feel pain or tenderness.
Over time, repetitive loading or compression of these tendons can lead to microscopic damage and thickening of the tendon.
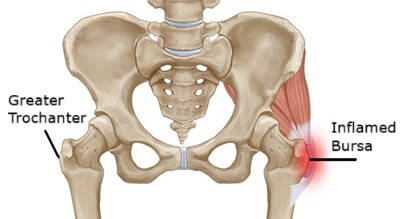
In some cases, gluteal tendinitis can also be accompanied by inflammation of the trochanteric bursa, a small fluid-filled sac that sits over the greater trochanter and helps reduce friction between the bone and the gluteal tendons.
This is known as trochanteric bursitis. When both are structures are affected, the condition is referred to as Greater Trochanteric Pain Syndrome (GTPS).
While the terms gluteal tendonitis or tendinitis imply inflammation, gluteal tendinopathy is a broader and more accurate term that reflects both early inflammatory and chronic degenerative changes in the tendon structure.
Gluteal Tendinitis Causes
Gluteal tendinopathy is typically caused by repetitive overloading or compression of the gluteal tendons. Common causes include:
- Repetitive overuse from activities like walking, hiking, running, lunging or stair climbing, especially on cambered or uneven surfaces
- Sudden increase in activity levels, such as starting a new exercise routine or returning to sport after time off
- Abnormal biomechanics, such as hip drop or excessive trunk sway during walking or running, and postural habits such as hip hanging
- Muscle imbalances, particularly weak glutes and tight hip flexors or ITB
- Age-related changes, especially in post-menopausal women, where tendon resilience may reduce
- Obesity, as excess weight places more strain on the tendons
- Gender – gluteal tendinitis is 4x more common in women than men
- Fall – landing on the greater trochanter can lead to gluteal tendinopathy
Gluteal Tendinopathy Symptoms
The most common symptom of gluteal tendinopathy is pain on the outside of the hip which may extend down the outer thigh towards the knee, especially when:
- Lying on the affected side
- Walking, particularly uphill or upstairs
- Standing on one leg e.g. when getting dressed
- Sitting cross-legged
- Getting up after prolonged sitting or inactivity
Other common symptoms of gluteal tendinopathy include:
- Tenderness over the outer hip, especially at the greater trochanter
- Weakness in the affected hip, especially when standing or walking. Weakness is usually bilateral and on average, the glutes are 32% weaker on the affected side and 23% weaker on the non-symptomatic side with gluteal tendinitis
- Pain with resisted hip abduction
- Stiffness or tightness around the hip, especially after rest causing reduced hip range of motion
- No obvious swelling or bruising unless trochanteric bursitis is also present
Gluteal tendinopathy pain is often described as a dull ache that becomes more intense over time with sharp, stabbing pain with certain movements.
How To Diagnose Gluteal Tendinopathy
A diagnosis of gluteal tendinitus is usually made through a combination of your clinical history, a physical examination, and, if needed, imaging tests.
A physiotherapist or doctor will:
- Ask about your symptoms, lifestyle, activity levels and aggravating factors
- Palpate the outside of your hip to locate tenderness
- Test hip abduction strength and range of movement
- Perform provocation tests such as the single-leg stance test, resisted external rotation or Faber test
- Observe your walking or running gait to assess pelvic control
While not always necessary, imaging can help rule out other causes or confirm the diagnosis of gluteal tendonitis:
- Ultrasound can show tendon thickening or partial tears
- MRI provides detailed images of both tendons and bursa
- X-ray may be used to rule out arthritis or bony changes
Differential Diagnosis
Other conditions can mimic gluteal tendinopathy symptoms, so it is important to rule out:
- Trochanteric Bursitis: often occurs alongside gluteal tendonitis and is often associated with localised swelling
- Hip Osteoarthritis: usually also causes groin pain and stiffness
- Iliotibial Band Syndrome: pain usually extends down the outer thigh to the knee
- Lumbar Referred Pain: from nerve irritation in the lower back
#CommissionsEarned from Amazon on qualifying purchases
Gluteal Tendinopathy Treatment
The aim of treatment for gluteal tendonitis is to reduce tendon load and irritation, correct biomechanics, and build strength gradually. Gluteal tendonitis treatment usually consists of a combination of:
1. Activity Modification
Avoid or reduce activities that aggravate symptoms, especially those involving prolonged standing and stair climbing.
Avoid positions that compress the tendon, like crossing your legs when sitting, lying on the affected side or standing with the hip “hanging” to one side e.g. when holding a young child on your hip
Use a pillow between your knees at night if lying on your side
Ensure you have rest days between training sessions to give the tendons time to recover
2. Ice, Heat and Pain Relief

Apply ice packs to the outer hip for 15–20 minutes several times a day during acute flare-ups of gluteal tendonitis to reduce pain and inflammation.
Some people find using heat packs is more effective, especially in chronic cases of gluteal tendinopathy. Over-the-counter anti-inflammatories like ibuprofen can help manage pain in the short term.
3. Physiotherapy
Physical therapy is an essential part of treatment for gluteal tendinitis to reduce pain and restore function.
It will usually involve a combination of:
- Manual Therapy: deep transverse friction massage, dry needling and joint mobilisations may be used to reduce muscle tension, joint stiffness and improve mobility
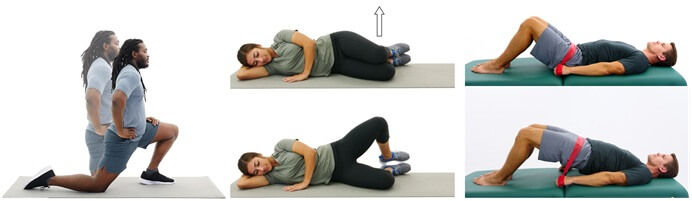
- Isometric Exercises: start with static exercises where the muscle is activated without shortening to strengthen and reduce pain without aggravating the tendons. E.g. sit with your knees bent and hip width apart, and your feet together. Squeeze your heels together for 10-20 seconds, 3 -5 times
- Glute Strengthening: especially targeting gluteus medius and minimus to offload the tendon. Exercises such as bridges, side-lying leg lifts and clamshells are particularly effective, but should only be done once pain-free.
- Progressive Loading: gradually work the muscles harder to gain more strength and stability such as resistance band walks and single-leg balance work
- Movement Retraining: to correct poor gait or pelvic control
Avoid stretching the glutes or ITB initially as that increases the compression force through the greater trochanter. But once symptoms have settled, it important to do glute stretches and ITB stretches to prevent the condition returning.
4. Injections
In some cases, corticosteroid or PRP (platelet-rich plasma) injections may be considered. Steroids reduce inflammation short-term, but repeated use can weaken tendons. PRP aims to support tendon healing using growth factors from your own blood.
5. Gluteal Tendinopathy Surgery
Surgery for gluteal tendinopathy is rare and only considered when symptoms are severe and unresponsive to at least 6 months of conservative treatment. Procedures may involve tendon repair, debridement, or bursectomy. Post-op rehab is essential for recovery.
Gluteal Tendinitis Recovery
Recovery times with gluteal tendonitis can vary depending on how long the problem has been present. With a consistent rehab program:
- Mild cases of gluteal tendonitis may settle in 6–8 weeks
- Moderate cases of gluteal tendinitis can take 3–6 months
- Chronic or recurrent cases of gluteal tendinopathy may take 6–12 months
Sticking to your rehab plan, avoiding aggravating positions, and slowly building strength are key to full recovery. It is important to stay active, but avoid “pushing through” pain.
FAQs: Gluteal Tendinopathy
What
Is The Fastest Way To Heal Gluteal Tendinopathy?
What Is The Fastest Way To Heal Gluteal Tendinopathy?
The fastest way to heal gluteal tendinitis is through early diagnosis, targeted physiotherapy, and avoiding aggravating activities. Strengthening the gluteal muscles, improving hip control, and modifying movements are key to speeding up recovery.
What Aggravates Gluteal Tendinopathy?
What Aggravates Gluteal Tendinopathy?
Aggravating factors include prolonged standing, walking, climbing stairs, lying on the affected side, and crossing your legs. Any activity that compresses the outer hip can worsen symptoms.
Can Gluteal Tendinopathy Be Cured?
Can Gluteal Tendinopathy Be Cured?
Yes, with the right treatment plan, most people fully recover from gluteal tendonitis. It may take several weeks or months depending on severity, but early intervention leads to the best outcomes.
How Long Does Gluteal Tendinopathy Take To Heal?
How Long Does Gluteal Tendinopathy Take To Heal?
Recovery typically takes between 6 weeks and 6 months. Chronic cases may take longer. Committing to a rehab program is essential for a full and lasting recovery.
Is Walking OK With Gluteal Tendinopathy?
Is Walking OK With Gluteal Tendinopathy?
Walking short distances is often okay with gluteal tendonitis, but avoid long walks or hills if they aggravate pain. Modify your gait to avoid hip drop or excessive leg crossing, and gradually increase walking tolerance under the guidance of your physiotherapist.
Does
Gluteal Tendinopathy Show Up On MRI?
Does Gluteal Tendinopathy Show Up On MRI?
Yes, MRI can reveal tendon degeneration, inflammation, or associated bursitis. It’s one of the best imaging tools for assessing the extent of tendon damage.
Are
There Gluteal Tendinopathy Exercises To Avoid?
Are There Gluteal Tendinopathy Exercises To Avoid?
Yes, in the early stages avoid exercises that place pressure through the greater trochanter such as glute stretches and ITB stretches. Clam strengthening and side leg lifts should only be done if they don’t aggravate gluteal tendinopathy symptoms.
Gluteal Tendinopathy Summary
Gluteal tendinopathy, also known as gluteal tendonitis or gluteal tendinitis, is a common cause of outer hip pain, especially in middle-aged women and runners. It is caused by excessive overloading or compressing of the gluteus medius or minimus tendons at the greater trochanter and is often associated with trochanteric bursitis.
Symptoms of gluteal tendonitis typically include pain on the outside of the hip, worsened by walking, climbing stairs, or lying on your side.
Treatment focuses on gluteal strengthening, activity modification, physiotherapy, and in some cases, shockwave or injection therapy. Most people recover well with early intervention and consistent rehab.
If you think you may have gluteal tendinitis, don’t ignore the signs. The earlier you address it, the easier it is to treat and the better your chances of a full recovery.
You may also be interested in the following articles:
- Outer Hip Pain
- Front Hip Pain
- Inner Hip Pain
- Hip Tendonitis
- Hip Strengthening Exercises
- Hip Pain Diagnosis Charts
Related Articles
Last Updated: September 12th, 2025
Next Review Due: September 12th, 2027