- Home
- Common Knee Conditions
- Bipartite Patella
Bipartite Patella Syndrome
Written By: Chloe Wilson, BSc(Hons) Physiotherapy
Reviewed by: KPE Medical Review Board
Bipartite patella syndrome is a condition where the kneecap is made up of two separate bones, instead of one, that have failed to fuse together during childhood. It is a rare condition, affecting only 1-2% of the population.
In most cases, it doesn’t cause any problems and may go completely unnoticed – it is often only discovered when an x-ray is done for an unrelated knee problem.
However, in some instances it can cause pain at the front of the knee, particularly when squatting down, and can limit function.
Here, we will look at what causes bipartite patella syndrome, how they are classified, the symptoms that can develop and how to treat them.
What Causes Bipartite Patella?
Bipartite patella is caused by the kneecap failing to form properly during childhood.
The patella, or kneecap, is a triangular shaped bone. When you are born, there is essentially no bone in the kneecap – it is made up of cartilage and blood vessels. During early childhood, as you grow, the kneecap cartilage gradually expands.
At around age 4, the cartilage starts to ossify, forming small portions of bone. These bone segments gradually fuse together and by the age of 12 a single kneecap has usually formed.
Occasionally, the bones fail to fuse completely leaving two distinct pieces of bone. There tends to be one large piece of bone and one smaller fragment.
This is what is known as bipartite patella and no one really knows why it happens. The two portions of bone remain unfused, connected by fibrocartilaginous tissue known as synchondrosis.
Bipartite patella is more common in males with a male:female ratio of 9:1.
Types Of Bipartite Patella
The first classification system for bipartite patella was introduced in 1921 by Saupe. He used the location of the fragment to classify the condition into three types of bipartite patella:
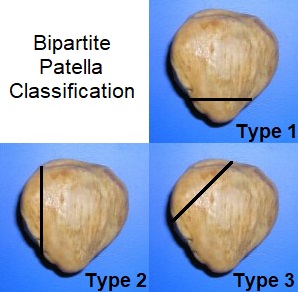
- Type 1: The fragment is at the inferior (bottom) portion of the patella. Incidence approximately 5%
- Type 2: The fragment is found on the lateral margin (outer side) of the patella. Incidence approximately 20%
- Type 3: The bone fragment is at the superolateral (upper, outer) portion of the patella. Incidence approximately 75%
So as you can see, by far the most common place to have the synchondrosis is at the top of the kneecap, on the outer side, type 3. In just under half of all cases of bipartite patella, both kneecaps are affected.
Bipartite Patella Symptoms
In approximately 98% of cases of bipartite patella, people are completely asymptomatic. This means there are no obvious signs that the kneecap hasn’t fully fused and the bipartite patella doesn’t cause any problems. In most cases, the condition is only discovered when the knee is x-rayed or scanned following an unrelated injury.

However, in 2% of cases, bipartite patella does go on to cause problems. This usually happens when the cartilage tissue between the bones, the synchondrosis, is damaged, causing irritation and inflammation. This is usually from a direct blow to the front of the knee, a fall or repetitive overloading at the knee.
Activities that typically cause problems with bipartite patella are those where there is repetitive knee bending, jumping or squatting such as with skiing, cycling, hill walking or basketball.
The most common symptoms that people experience with symptomatic bipartite patella are:
- Knee Pain: usually at the top of the patella on the outer side of the knee. It tends to be worse with squatting activities as more force goes through the kneecap
- Tenderness: when pressure is placed over the bony fragment
- Knee Swelling: this tends to be fairly localised
- Instability: the knee may feel like it is going to give way
- Bony Ridge: you may be able to feel a slight ridge on the patella
- Large Patella: The kneecap may well be larger than usual
Diagnosing Bipartite Patella
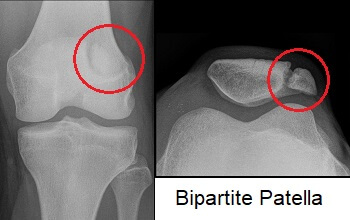
The unfused area of the kneecap in bipartite patella usually shows up clearly on an x-ray or MRI scan of the knee. The triangular bone will have a gap in it where the fibrocartilaginous tissue has failed to ossify.
It may initially be mistaken for a patella fracture but the tell-tale signs of bipartite patella are:
- Rounded Edges: Rather than the characteristic jagged edges seen in patella fractures
- Location: A gap on the superolateral aspect of the kneecap is characteristic of bipartite patella rather than a fracture
- Bilateral: If both knees show similar findings on x-ray it is most likely bipartite patella rather than a fracture
#CommissionsEarned from Amazon on qualifying purchases
Treatment Options
Treatment for bipartite patella usually consists of:
1. Rest
It is important to rest from all aggravating activities with bipartite patella. If an activity causes pain, don’t do it. The joint needs time to settle down so it can heal. LEARN MORE >
2. Ice

Regularly applying ice to the knee can help to reduce inflammation in the synchondrosis and thus reduce kneecap pain. In the ice treatment section you can find our top tips on how to apply ice safely and effectively.
3. Exercises
It is really important to strengthen and stretch the knee muscles to allow the kneecap to move properly without the synchondrosis getting irritated and inflamed. With bipartite patella you want to do a combination of:
- Knee Stretches: to reduce tension in the muscles and take the pressure of the patella
- Knee Strengthening Exercises: to improve the strength and function at the knee
- Kneecap Exercises: to improve the positioning and movement of the kneecap
4. Knee Brace
Another thing that can help is to wear with bipartite patella is a knee brace to unload the kneecap and reduce the force going through the synchondrosis. Knee Straps can be particularly helpful.
In some cases the knee may be immobilised in a brace that holds the knee in 30 degrees of flexion. Visit the knee braces section to find the right brace for you.
5. Steroid Injections
Your doctor may give you an injection of corticosteroid mixed with local anaesthetic to reduce pain and inflammation with bipartite patella. The knee usually feels instantly better but the effects can be short-lived. You can find out all about how steroid injections work and the possible side effects in the knee injections section.
6. Medication
Your doctor may prescribe painkillers e.g. paracetamol/Acetaminophen and anti-inflammatory medication e.g. ibuprofen/Advil to help to reduce any knee pain and inflammation with bipartite patella. Always check with your doctor before taking new medications.
7. Physical Therapy
Regular session of physical therapy can also be helpful to reduce pain and inflammation with bipartite patella and to address any areas of muscle weakness around the knee. Your physical therapist will work on a rehab program with you of strengthening and stretching exercises and may also use ultrasound to help reduce inflammation and improve healing.
The symptoms of bipartite patella usually settle after two or three months with these treatment methods. However if they persist for more than six months then your doctor may advise surgery.
Surgical Treatment
There are three surgical options with bipartite patella:
- Open Excision: this is when the smaller fragment of bone is removed. This is the most common surgical treatment technique for bipartite patella
- Open Reduction Internal Fixation (ORIF): A screw is inserted to hold the bone fragments together. This tends to be done for larger fragments
- Lateral Release: If there is tightness in the lateral retinaculum or vastus lateralis that is pulling the patella out of alignment, then the tight structures are cut to allow the kneecap to sit centrally. You can find out more about what surgery involves and the recovery process in the lateral release section.
People usually make a full recovery from bipartite patella surgery within a few months and are able to get back to their usual activities. It is important to do both strengthening and stretching exercises for the first few months to ensure you regain full strength and mobility in the knee.
If there are no symptoms associated with bipartite patella, then no treatment is required, it is better to just leave it alone.
What Else Can Help?
There are a number of other conditions that are more likely to cause pain at the front of the knee including:
You can find out more about each of these and other possible causes in the front knee pain section.
Bipartite patella is a rare condition, and of those who do have it, most will go through life completely unaware they have the condition.
Page Last Updated: 03/02/24
Next Review Due: 03/02/26